
Research Summary: Treatment Decision Making in Adults with Cleft
Background
As part of the Adults Services Programme, 2018 saw CLAPA launch the ‘Whole of Life’ Survey, a comprehensive questionnaire for adults in the UK born with a cleft.
We know that cleft lip and/or palate impacts people’s health, but we also recognise that the experiences of the treatment itself can impact people in many different ways. We were interested to learn more about people’s experiences of cleft treatment and how this may influence their attitudes towards future treatment.
The ‘Whole of Life’ survey included a couple of sections that asked about people’s experiences with their surgical, dental and psychological treatment. The results of this part of the survey fed into an academic paper published in the Cleft Palate Craniofacial Journal (CPCJ).
This paper was authored by Kenny Ardouin, Adult Services Manager at CLAPA, Dr Nicola Stock, Centre for Appearance Research, David Drake, Cleft Surgeon, Scottish Cleft Service and Sandip Popat, Restorative Dentist, Spires Cleft Service.
We’ve summarised the findings of this paper below.
We’ll be discussing the findings of this paper and what they mean for the cleft community in more detail on Monday 14th June at 8 pm. Follow us on Facebook, Twitter or Instagram to find out more and join the discussion.
Surgical Experiences
The most common surgery that people had in adulthood was a rhinoplasty (53% of operations), followed by orthognathic jaw surgery (23% of operations).
19% of operations were to help with speech concerns, while 7% were to repair a persistent hole (also known as a fistula) in the palate, and 5% of operations were a secondary lip revision.
Most people reported being happy with their surgical experiences. The majority strongly agreed with the statements “Overall, I am happy with the surgical outcomes from my cleft treatment” and “overall, I am pleased with the surgical care and follow up that I received”.

Dental, Orthodontics and Restorative Dentistry
77% of people completing our survey had visited a General Dental Practitioner (GDP) within the 12 months before completing the survey. 12% had visited between 1-2 years ago, while the remainder had visited more than 2 years ago. 3% could not remember the last time they visited a GDP, and 1% hadn’t visited for more than 10 years.
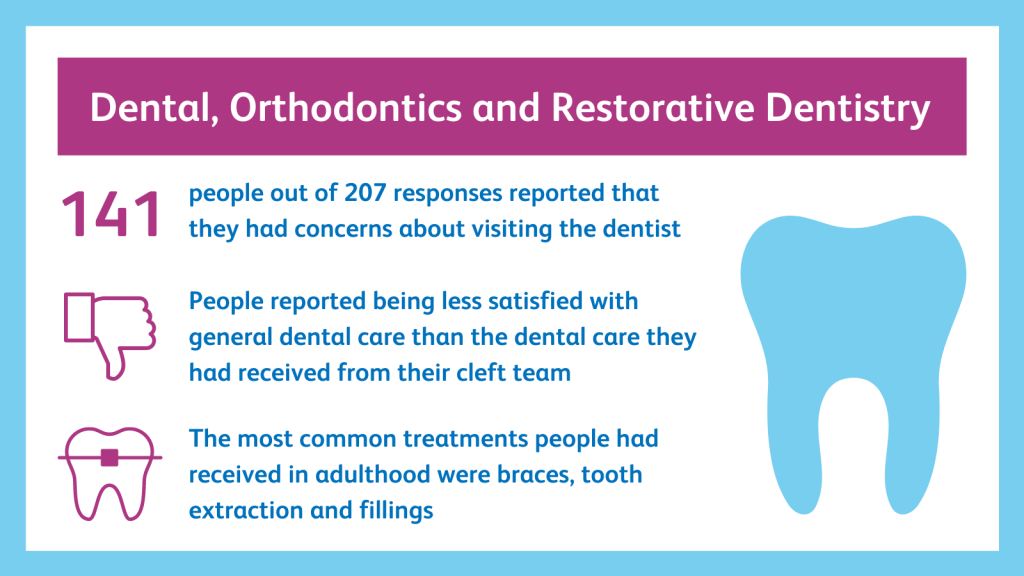
Of the 207 people who completed the survey, 141 (68%) reported having concerns about visiting the dentist.
The main concerns were:
- The cost of dental care (56%)
- Fear or anxiety (50%)
- Pain or sensitivity (39%)
- Concerns that their dentist wouldn’t understand cleft (34%)
- Having had a prior bad experience (21%).
People reported being considerably less satisfied with general dental care from a GDP than the dental care they had received from their cleft team.
Receiving cleft-related orthodontics and/or restorative dentistry work in adulthood was very common. The most common treatment was braces (experienced by 83%), tooth extractions (80%) and fillings (74%). One in four people had seen a restorative dentist or orthodontist for dentures. People generally reported a high level of satisfaction with the cleft team’s dental services.
Ongoing Surgical Concerns and Desire for Further Treatment
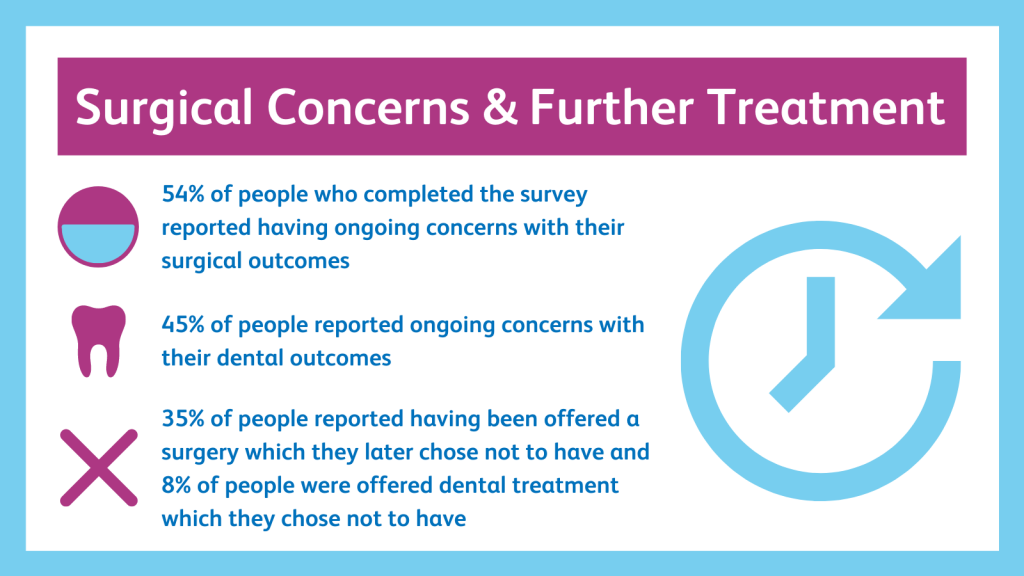
54% reported having ongoing concerns with their surgical outcomes. These were most commonly around facial asymmetry, lip scarring, breathing/sinus issues, difficulties with eating and drinking, and pain or numbness. People gave mixed responses to whether or not they would consider having further surgery, and were slightly more likely to consider having further surgery to address functional concerns like breathing than to change their appearance.
45% of people reported ongoing concerns with their dental outcomes. These were most commonly that previous dental work is failing, teeth are not straight, or missing or loose teeth. People were more likely to agree to further dental treatment than surgery, and were just as likely to undergo dental work to change their appearance as for functional concerns.
35% of people reported having been offered a surgery which they later chose not to have. 8% of people were offered dental treatment, which they chose not to have. The most common reasons for refusing a procedure were that people felt happy with their current appearance and/or function, that the costs outweighed the benefits, that the desired outcome wasn’t guaranteed, or that they had had enough of surgery.
Awareness of Entitlement to NHS Services
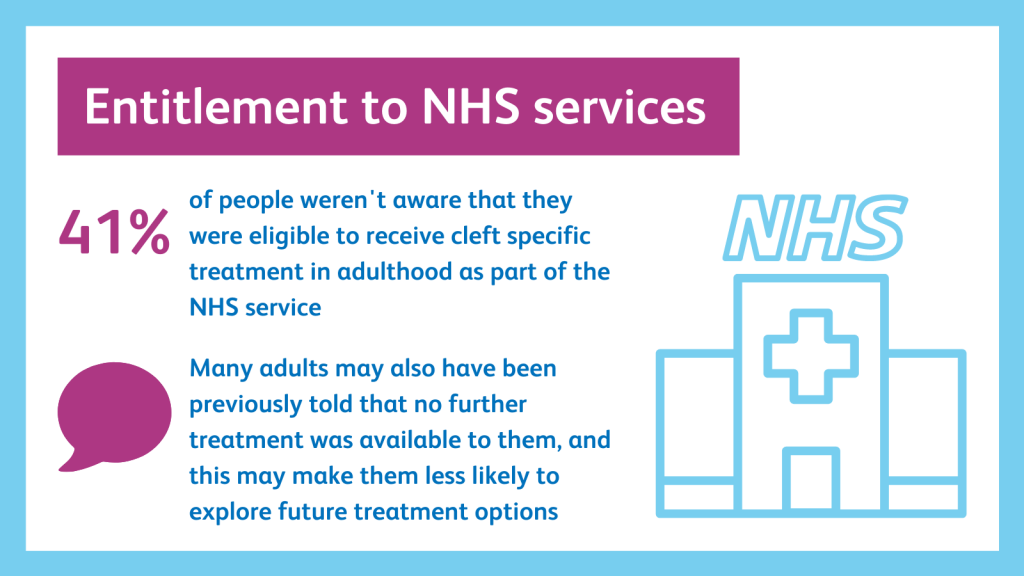
41% of people weren’t aware that they were eligible to receive cleft specific treatment in adulthood as part of the NHS service.
Sadly, 17% of people had paid privately for cleft related treatment that would have been available on the NHS; this was most frequently dental/orthodontic or restorative dentistry work.
41% of people had concerns that their eligibility to access cleft services may change in the future. A considerable number of people had reported great difficulty in accessing the cleft team when they needed it due to difficulties obtaining a referral.
Many adults may also have been told at a previous point in time that no further treatment was available to them, and this may make them less likely to explore future treatment options when faced with new or ongoing concerns relating to their cleft.
Conclusions
In summary, adults in the UK who were born with a cleft may experience ongoing issues related to their surgical care and their general dental, orthodontic and/or restorative dentistry outcomes. However, adults may be reluctant or unable to re-engage with the cleft care system due to previous traumatic experiences, concerns about anxiety, fear, pain or cost, or difficulties accessing a referral. It is also likely that there is a considerable proportion of the adult cleft population who have been turned away from cleft services in the past, and are unaware that they are entitled to care.
To address these issues, it is recommended that information is given to young adults who are about to complete their routine cleft treatment. The CLAPA Leavers’ Pack hopes to address this problem.
Additionally, it is recommended that health professionals ensure that patients have the same expectation as they do of what treatment will achieve. This can be achieved through patient reported outcome measures/questionnaires. Given that many people reported having experienced traumatic experiences around treatment earlier in life, it is also recommended that support from psychology services is routinely offered when adults return to the cleft service later in life.
It is recommended that education for patients of all ages be provided around treatment options, including dentistry and jaw surgery. These topics and others can be found in our Cleft Talk series.
Check out our Q&A session where we unpacked the findings further and explained how we are using what the community told us to ensure people’s social and interpersonal experiences are well supported from birth through adulthood.


